Chronic Venous Insufficiency:
Symptoms & Treatment Guide
About Varicose Veins
Do your legs feel swollen, heavy, or sore by the end of the day? Have you noticed more visible or painful veins? These might be signs of chronic venous insufficiency (CVI), a condition where blood has a hard time flowing back to your heart from your legs.
At the Vascular and Interventional Clinic in Singapore, our team helps people understand and manage chronic venous insufficiency with a focus on personalized care and proven treatments.
Keep reading to find out more about this condition, including symptoms, how it develops, treatment options, and costs.
What
What Is Chronic Venous Insufficiency?
Recurrence happens when underlying issues aren’t fully addressed. Here’s what you should understand.
What Is Chronic Venous Insufficiency?
Chronic venous insufficiency happens when the veins in your legs can’t pump blood back to your heart as they should. This condition builds up over time and messes with normal blood flow in your legs, leading to symptoms that can really affect your daily life.
This occurs when the little valves in your leg veins get damaged or weak. These valves usually work like one-way doors, letting blood move up toward the heart and stopping it from going back down. If they fail to do their job, blood can pool in your legs, which causes pressure to rise in the veins.
Are Varicose Veins a Sign of Poor Circulation or Health Issues?
Varicose veins do indicate compromised venous circulation, but they don’t necessarily reflect overall poor health. The relationship between varicose veins and systemic health is more nuanced than many people realise.
Venous insufficiency is the primary circulation problem associated with varicose veins. This occurs when vein valves become damaged or weak, allowing blood to pool in the legs rather than efficiently returning to the heart. This is a localised circulation issue rather than a systemic cardiovascular problem.
However, many healthy, active individuals develop varicose veins due to genetic factors alone. Having varicose veins doesn’t indicate heart disease, diabetes, or other serious systemic conditions in most cases.
When to be concerned: Varicose veins may indicate more serious health issues if they’re accompanied by leg swelling, skin changes, persistent pain, or a history of blood clots. These symptoms warrant comprehensive vascular evaluation.
Key Differences between Chronic Venous Insufficiency and Varicose Veins
Chronic Venous Insufficiency
- A condition where the veins struggle to send blood back to the heart.
- Caused by weakened or damaged vein valves.
- May not always have visible signs on the skin in early stages.
- Symptoms can include leg heaviness, swelling, aching, or skin discolouration.
- Can lead to varicose veins over time.
Varicose veins
- Twisted, enlarged veins visible just under the skin, often blue or purple.
- Typically a symptom of underlying chronic venous insufficiency.
- More of a visual and cosmetic sign than a functional issue on its own.
- Often appear on the legs, especially after standing for long periods.
- May be painless or cause aching, itching, or discomfort.
Stages
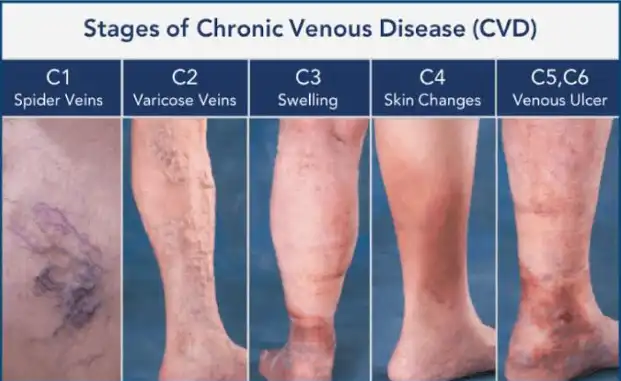
The 6 Stages of Chronic Venous Insufficiency
Knowing the progression of chronic venous insufficiency can help you figure out where you might be in the process. The medical community uses a system called CEAP (Clinical, Etiological, Anatomical, Pathophysiological) to classify the six stages of this condition, from mild to severe.
Stage 0 – No Visible Signs (But Symptoms May Exist)
In Stage 0, your legs might look fine, but you could already feel symptoms of CVI. Typical signs include leg heaviness, aching, or tiredness, especially after standing or sitting for a while. Some people also have restless legs or cramps at night.
This stage can be tough since others may not understand your discomfort when your legs look normal. But these early symptoms are important warnings that your vein valves are struggling.
Stage 1 – Spider Veins & Mild Swelling
At Stage 1, you’ll start seeing the first signs of chronic venous insufficiency. This includes spider veins – small, thin veins that can be red, blue, or purple. You might also experience mild swelling in your ankles or feet, especially by the end of the day.
The swelling often goes down overnight or when you elevate your legs, but comes back as the day goes on.
Stage 2 – Varicose Veins & Leg Heaviness
In Stage 2, larger varicose veins start to show up. These twisted, bulging veins will be more noticeable. You’re likely to feel more leg heaviness, aching, and fatigue.
The discomfort usually gets worse throughout the day but can improve with leg elevation or walking. Many people look for treatment at this stage since symptoms begin to interfere with daily life.

Stage 3 – Swelling (Oedema) & Skin Discoloration
Stage 3 brings persistent swelling that doesn’t entirely go away even with rest or elevating your legs. This swelling, known as oedema, mainly affects your ankles, feet, and lower legs. You might also notice skin discoloration, often a brown or reddish tint around your ankles and lower legs.
This occurs because blood cells leak from damaged veins and break down in your tissues, leaving behind iron deposits.
Stage 4 – Skin Changes (Lipodermatosclerosis, Eczema)
In Stage 4, more serious skin changes occur. You might develop lipodermatosclerosis, where the skin and underlying tissues get thick, hard, and woody. Some people also deal with venous eczema, leading to itchy, inflamed, and sometimes weeping patches of skin.
These changes can be uncomfortable and make you feel self-conscious.
Stage 5 – Healed Venous Ulcers
Stage 5 means you’ve had venous ulcers before, but they’ve healed. These ulcers usually occur around your ankles and can take a long time to heal.
Even though they’re healed, chronic venous insufficiency is still an issue, and there’s a high chance of the ulcers coming back without ongoing treatment.
Stage 6 – Active Venous Ulcers (Most Severe)
Stage 6 is the most severe form of chronic venous insufficiency, marked by active venous ulcers which are open wounds around the ankles that can be very painful. They can be hard to heal due to poor circulation and high pressure in your leg veins.
These ulcers can become infected and may need specialised wound care in addition to treatment for the underlying CVI.
when to worry
Symptoms & Warning Signs of Chronic Venous Insufficiency
The symptoms usually build up gradually and might seem small at first, but typically get worse over time without proper care.
What Do Legs Look Like with Venous Insufficiency
As chronic venous insufficiency progresses, you’ll start seeing changes in your legs. The typical visual signs include:
- Spider veins – small red or blue veins that look like webs on thighs, calves, or ankles
- Varicose veins – larger, twisted veins that bulge from the skin
- Leg swelling (oedema) – especially noticeable at the ankles and feet, usually worse by the end of the day
- Skin discoloration – brownish or reddish tint around the ankles
- Skin texture changes – dry, itchy, or flaky skin in the affected areas
These visible changes usually happen gradually, starting with spider veins and moving to more noticeable varicose veins and skin changes if left untreated.
Early Warning Signs of Chronic Venous Insufficiency
The earliest signs of chronic venous insufficiency often relate more to how your legs feel rather than how they look. Common warning signs include:
- Leg heaviness and fatigue – especially after being on your feet or sitting for long periods
- Aching or throbbing pain that gets better with elevation or movement
- Night-time leg cramps that disrupt your sleep
- Restless leg sensation – a feeling that you need to stretch or move your legs
- Leg discomfort that gets worse throughout the day and eases with rest
These symptoms build over time and can worsen without proper management.
Symptoms of Poor Blood Circulation in the Legs
Poor circulation from chronic venous insufficiency leads to several noticeable symptoms that can affect your comfort:
- Temperature changes – legs may feel cold or numb, even in warm weather
- Tingling sensations – the feeling of pins and needles in your legs or feet
- Skin issues – dry, itchy, or flaky patches on your legs
- Slow healing – cuts taking longer than usual to heal
- Burning sensation – uncomfortable burning feeling in the legs or feet
- Activity-related relief – symptoms improving with movement
These circulation symptoms typically worsen during the day, especially if you’ve been inactive.
Causes
What Causes Chronic Venous Insufficiency?
Knowing what leads to chronic venous insufficiency helps you recognise your risk factors and take steps to prevent it from getting worse. This condition develops due to a combination of factors that damage the valves in your leg veins over time.
Faulty Vein Valves & Poor Circulation Explained
Your leg veins have tiny valves that act like one-way doors, allowing blood to flow up towards your heart while preventing it from going backward. These valves are essential because they help blood fight against gravity. If they become damaged or weakened, they can’t close properly, causing blood to flow backward and pool in your legs. This builds pressure in your veins, stretching the walls and damaging more valves, making the problem worse over time.
Damage to these valves can result from normal wear over time or specific incidents like blood clots, injuries, or extended periods of pressure in your legs.
Other Causes
Jobs That Worsen Chronic Venous Insufficiency
Certain jobs increase the risk of developing chronic venous insufficiency because they require long periods of standing or sitting. High-risk professions include:
Prolonged Standing Jobs:
- Nurses and healthcare workers
- Teachers and lecturers
- Retail assistants
- Factory workers
- Hairdressers
- Security personnel
Prolonged Sitting Jobs:
- Office workers
- Professional drivers (taxis, trucks, buses)
- Airline pilots and crew
- Call center operators
- IT professionals
If your job requires long hours of standing or sitting, taking regular breaks, wearing compression stockings, and doing simple leg exercises can help lower your risk.
Diabetes, Obesity & Other Risk Factors
A few health conditions and lifestyle choices can raise your risk of developing chronic venous insufficiency, such as:
Medical Conditions:
- Diabetes – high blood sugar levels harm blood vessels and circulation
- Obesity – extra weight puts pressure on leg veins, limiting movement
- Previous blood clots – can damage vein valves and increase risk
- Heart issues – affect overall blood flow
Demographic Factors:
- Age over 50 – veins naturally wear out over time
- Female gender – hormonal changes during pregnancy and menopause
- Family history – inherited tendencies to develop vein problems
- Pregnancy – increased blood volume and hormonal changes
Lifestyle Factors:
- Sedentary lifestyle – lack of exercise hurts muscle function
- Smoking – damages blood vessels and circulation
- Extended standing or sitting – increases pressure on leg veins
Treatment options
Chronic Venous Insufficiency Treatment Options by Stage in Singapore
Treatment options for chronic venous insufficiency depend on your condition stage and personal circumstances. Early intervention can prevent it from progressing, while advanced cases may need more invasive treatments.
Early Stages (0-1): Compression Stockings & Lifestyle Changes
In the early stages of chronic venous insufficiency, conservative treatments usually work well. Compression stockings are often the first go-to, applying pressure to your legs that’s strongest at the ankles and gradually lessens as it goes up.
Lifestyle changes are just as crucial. Regular exercises like walking, swimming, or cycling can boost circulation. Elevating your legs when resting, maintaining a healthy weight, and avoiding long stretches of standing or sitting can help manage symptoms and stop progression.
Moderate Stages (2-4): Minimally Invasive Treatments (RFA, Sclerotherapy)
Once chronic venous insufficiency progresses to moderate stages, minimally invasive treatments become more suitable.
Radiofrequency ablation is popular as it uses heat to seal off damaged veins and reroute blood to healthier ones. Sclerotherapy is also effective for both spider veins and smaller varicose veins.
These procedures usually happen as outpatient treatments, with minimal downtime. Most people can return to normal activities in a few days, although you’ll need compression stockings and should avoid heavy exercise for a short while.
Severe Stages (5-6): Wound Care & Surgery
For advanced chronic venous insufficiency with active or healed ulcers, comprehensive treatment becomes necessary to address both vein issues and wound care.
Good wound care is vital for healing ulcers and preventing infections. In severe cases, surgery might be needed, which could involve stenting to alleviate any narrowing, or removing badly damaged veins. The aim is to improve blood flow and lower the pressure causing ulcers.
lifestyle impact
Living with Chronic Venous Insufficiency
Chronic venous insufficiency affects more than just your physical health; it can take a toll on your daily life, emotional well-being, and overall quality of life.
What Happens If Venous Insufficiency Is Left Untreated?
If untreated, chronic venous insufficiency usually gets worse. The condition advances through the stages, leading to permanent skin changes, recurring ulcers, and greater pain or disability.
Untreated chronic venous insufficiency can also lead to more serious issues like blood clots, infections, and in rare cases, severe tissue damage. The longer you wait to seek treatment, the fewer options you may have and the harder it may become to get good results.
Yet, it’s never too late to start treatment. Even if you are in advanced stages, proper care can help manage symptoms, heal ulcers, and prevent further complications.
Can You Live a Long Life With Venous Insufficiency?
Many people worry that chronic venous insufficiency will affect their lifespan, but with proper management, you can live a normal, healthy life.
The condition itself isn’t life-threatening, although it can lead to complications if ignored. The key to living well with this condition is getting an early diagnosis and proper treatment.
By managing your symptoms, you can maintain an active lifestyle and continue enjoying a good quality of life.
How Chronic Venous Insufficiency Affects Daily Activities
Chronic venous insufficiency symptoms can make everyday tasks tough. Pain, heaviness, and swelling can make it hard to stand for long periods, affecting work and household chores.
You might avoid activities you used to love, like walking or sports. Visible changes in your legs can also make you self-conscious about wearing certain clothes, leading to lifestyle adjustments. Sleep might suffer too, as many deal with leg cramps or restlessness at night.
But with appropriate treatment and management, most people can get back to their usual activities and improve their quality of life.
FAQ about CVI
Does chronic venous insufficiency go away?
Chronic venous insufficiency is a progressive issue that doesn’t just disappear on its own. However, with the right treatment and care, you can keep the symptoms under control and prevent the condition from worsening. Early care often helps stop progression and relieve symptoms well.
Some treatments, like sclerotherapy or radiofrequency ablation, can permanently remove the problematic veins. But the tendency to develop vein issues may still exist, which is why ongoing management is key.
Can chronic venous insufficiency be cured?
There’s no cure that reverses all the damage from chronic venous insufficiency, but modern treatments can effectively manage it and eliminate many problematic veins.
The goal is to improve blood flow, relieve symptoms, and prevent progression.
Is walking good or bad for chronic venous insufficiency?
Walking is generally advised for those with chronic venous insufficiency. The rhythmic movement of your calf muscles helps pump blood back to your heart, boosting circulation in your legs. Regular walks can help reduce symptoms like swelling, heaviness, and pain.
Can chronic venous insufficiency lead to amputation if left untreated?
Amputation due to chronic venous insufficiency is very rare. Unlike arterial disease, which cuts off blood supply, CVI affects the return of blood to the heart instead of oxygen-rich blood delivery to your tissues.
However, untreated severe chronic venous insufficiency can lead to ulcers that may get infected. In rare cases, severe infections that don’t respond to treatment could lead to serious complications, but this is uncommon with modern medical care.
CONTENTS
YOUR Preferred Health Partner
Why Choose the Vascular & Interventional Centre
We Own Our Own Hybrid Operating Theatre
Unlike many other clinics, the Vascular & Interventional Centre owns and operates our own fully equipped day surgery theatre (angiosuite). This gives you a significant advantage:
- Lower facility and equipment fees – as we do not rely on third-party hospitals.
- Faster scheduling – skip the hospital queues, your procedure can be done promptly and at your convenience.
- Seamless care – from consultation to surgery and follow-up, all under one roof.
This integrated setup allows us to offer greater cost transparency, shorter waiting times, and a smoother overall experience for patients seeking varicose veins treatment.
Highly Experienced Team with Transparent Pricing
Our team brings years of specialised experience in varicose veins treatment, having successfully treated thousands of patients with various venous conditions.
We believe in transparent pricing without hidden costs or unexpected charges. Before beginning treatment, you’ll receive a detailed cost breakdown including all anticipated expenses, helping you plan accordingly and avoid financial surprises during your treatment journey.
Our commitment to transparency extends to treatment expectations, potential risks, and realistic timelines for results. We want you to feel confident and well-informed.
